Why Diabetic Retinopathy Needs Close Monitoring
Diabetic retinopathy is a complication of having diabetes. It affects the blood vessels in the retina and can cause permanent vision loss or blindness without treatment.
If you have diabetic retinopathy, ongoing monitoring, and prompt treatment is the best way to prevent further damage to your retina and preserve your remaining sight.
Keep reading to learn about diabetic retinopathy, why it needs constant monitoring, and the available treatment options.
What is Diabetic Retinopathy?
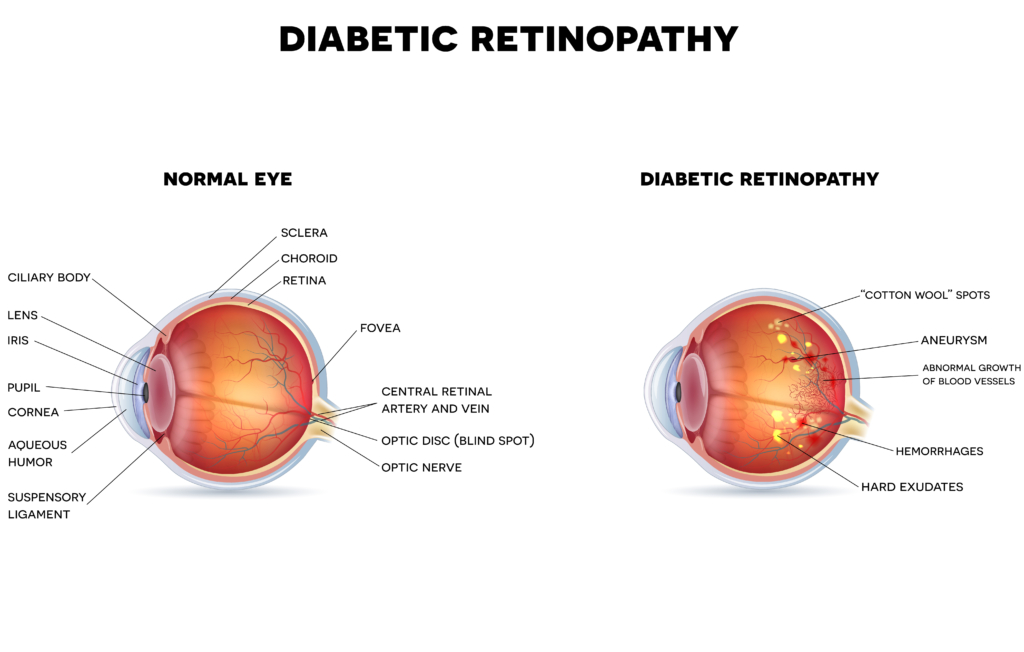
Diabetic retinopathy happens when too much sugar in the blood begins to damage the tiny blood vessels in your retina. The retina is the thin layer of tissue at the back of your eye that changes light into electrical signals.
These signals are then transmitted to the brain and converted into the images you see. Over time, the high blood sugar levels block the small vessels or cause them to leak.
When this happens, it leads to impaired blood circulation and bleeding. This may result in severe vision loss or blindness.
Types of Diabetic Retinopathy
In diabetic retinopathy, damage to the blood vessels in the retina happens in two main stages. These are:
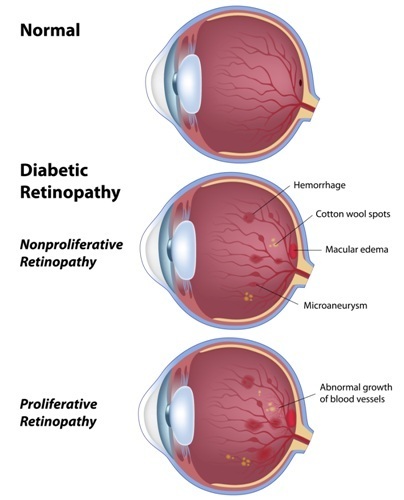
Non-Proliferative Diabetic Retinopathy
Non-proliferative retinopathy is the earliest stage of diabetic retinopathy. During this stage, the blood vessels weaken and form small bulges known as microaneurysms.
Microaneurysms may rupture and leak blood and fluid into the macula, causing swelling in the macula or macular edema. The macula is the central part of your retina.
It’s responsible for your sharp, straight-ahead vision. Sometimes, the blood vessels in your retina can also close completely, cutting off blood supply to the macula, a process called macular ischemia.
Proliferative Diabetic Retinopathy
Proliferative retinopathy is the advanced stage of diabetic retinopathy. In this stage, new blood vessels form on the retina’s surface, a process called neovascularization.
Neovascularization happens when your eyes try to replace damaged and closed-off blood vessels. However, the newly formed vessels are usually abnormal and weak.
Because they are weaker than blood vessels usually produced, these can easily burst and leak into the vitreous humor, completely blocking your vision. The vitreous is the gel-like substance that fills your eye.
Leaks from the fragile vessels can also result in scar tissue formation. In turn, scar tissue may tug on the retina and pull it away from the wall of your eye, causing a retinal detachment.
A retinal detachment is a medical emergency resulting in permanent vision loss if left untreated.
Symptoms of Diabetic Retinopathy
Diabetic retinopathy typically affects both eyes. You may develop diabetic retinopathy and not realize you have it.
During its early stages, there are few noticeable symptoms of diabetic retinopathy, making regular eye exams crucial. As the eye condition becomes more severe, you may have symptoms such as:

- Blurry vision
- Floaters
- Colors looking faded
- Poor night vision
- Vision that fluctuates from blurry to clear
- Dark or empty areas in your field of vision
- Eye pain
- Sudden vision loss
Causes of Diabetic Retinopathy
If you have diabetes, you’re at risk of developing diabetic retinopathy. Your risk of developing the eye condition becomes even higher if you:

- Have had diabetes for a long time
- Have poorly controlled blood sugar levels
- Are pregnant
- Have high cholesterol
- Have high blood pressure
- Smoke frequently
How to Monitor Diabetic Retinopathy

Even if you have your blood sugar under control, there’s still a possibility that diabetic retinopathy can progress and cause blindness. You must visit your optometrist or ophthalmologist regularly for close monitoring if you have diabetic retinopathy.
With careful monitoring, your optometrist or ophthalmologist can assess your retina health and determine if there have been any changes to your blood vessels or retinal damage. If there’s damage or change, your optometrist or ophthalmologist will provide timely treatment that can slow or prevent the progression of diabetic retinopathy.
Most patients require ongoing monitoring and treatment, increasing frequency as the condition advances.
How to Treat Diabetic Retinopathy
The treatment for diabetic retinopathy will depend on its stage and the extent of damage to the retina. For instance, you may not need treatment immediately if you have mild to moderate non-proliferative retinopathy.
Instead, your optometrist or ophthalmologist will monitor you frequently to determine when treatment is necessary. Here are some of the treatment options for diabetic retinopathy:
Anti-VEGF Injections
Anti-Vascular Endothelial Growth Factor or Anti-VEGF injections work by blocking the effects of VEGF. VEGF is the protein that encourages the growth of abnormal blood vessels in the retina.
The medications are directly injected into your eyes to stop or slow the growth of new vessels. With these injections, your optometrist or ophthalmologist can prevent vision loss and even improve vision in some cases.
You may require multiple anti-VEGF injections to control the growth of new vessels and protect your eyesight. The number of injections needed will depend on the severity of diabetic retinopathy and your response to treatment.
Laser Treatment
Laser treatment or photocoagulation is used to slow or prevent the progression of diabetic retinopathy. Your optometrist or ophthalmologist will use targeted laser energy to shrink blood vessels and seal leaking abnormal ones.
Shrinking and closing off these vessels slows or stops any leaking and buildup of blood and fluid. Consequently, this reduces the risk of further damage to your retina and protects against additional vision loss. You may require more than one treatment session, depending on the severity of diabetic retinopathy.
Vitrectomy
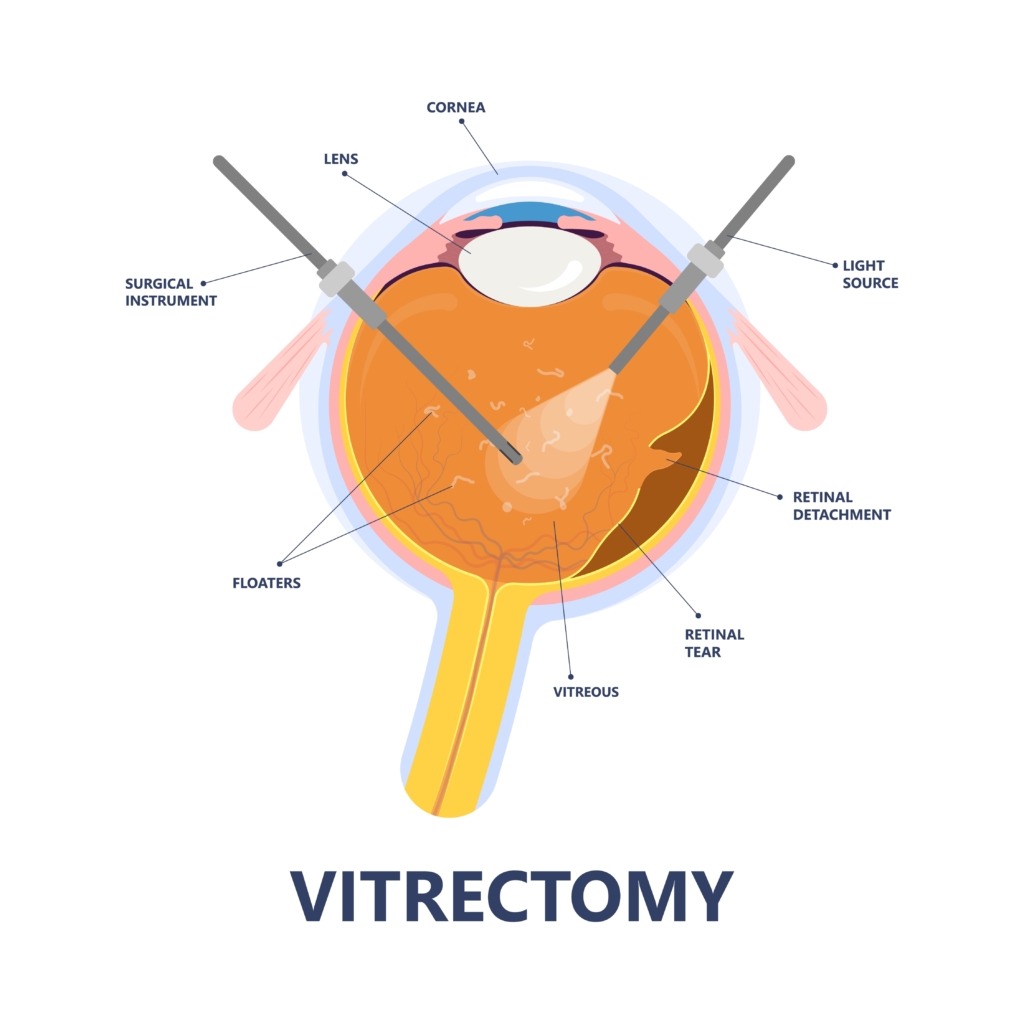
You may need a vitrectomy if you have advanced diabetic retinopathy. A vitrectomy can address complications like vitreous hemorrhage or retinal detachment and slow or stop the progression of diabetic retinopathy.
During the procedure, your surgeon will remove the vitreous mixed with blood and scar tissue. They will then use a transparent solution to replace the vitreous.
A vitrectomy can improve your vision and slow or stop further retinal damage.
Prevent Vision Loss from Diabetic Retinopathy
The expert optometrists and ophthalmologists at Eye Consultants of North Dakota can detect diabetic retinopathy even in its early stages. If you’re diagnosed with the condition, they will closely monitor your eyes and offer prompt treatment to save your sight.
Do you have diabetes and diabetic retinopathy? Schedule your appointment today at Eye Consultants of North Dakota in Fargo, ND, to learn more!



