How Do I Know If I Need a Corneal Transplant?
Have you recently been told that you’ll need a corneal transplant? You may have questions, including what to expect and why you need one.
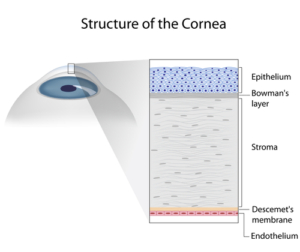
The cornea is the clear, front part of the eye that helps the eye bend light and focus. It also protects the inner eye from UV light and irritants like dust.
If you’ve suffered significant damage to the cornea, a corneal transplant may become necessary. Keep reading to learn more about corneal transplants!
What Health Problems Affect the Cornea?
Several conditions can make undergoing a corneal transplant necessary. You may suffer damage to the cornea due to permanent scarring, as well as develop vision loss.
Some health conditions that may affect the cornea include:
Dry Eye Syndrome
If your eyes regularly feel dry and gritty, you may have dry eye syndrome. This condition occurs if you don’t produce enough tears or the tears being produced are low in quality.
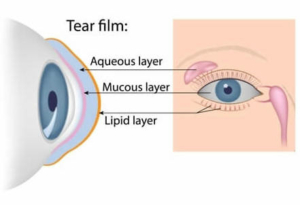
When this happens, there’s not enough oil to cover the cornea’s surface. The tear film has three components: water, oil, and mucus.
If any of these three components are missing, the tear film can’t provide the correct nutrients to the eyes through your tears. Having healthy tears is necessary if you want to be able to see clearly.
Without enough tears and oil, it may feel like you have sand or grit in your eyes. Many people who struggle with dry eye syndrome blink frequently to try to improve how their eyes focus. If left untreated, this chronic condition can damage the surface of the eye and require a corneal transplant.
Corneal Ulcers
Corneal ulcers are infections of the cornea. People who are immunocompromised or use contacts have the highest likelihood of developing these ulcers. The condition can also happen to people who have dry eyes or cannot fully close their eyelids.
These infections can cause permanent blindness as the bacteria attacks the cornea. Corneal ulcers require immediate treatment to keep your eyesight safe. A corneal transplant can remove cells damaged by the infection and restore any vision you may have lost.
Fuchs’ Dystrophy
Fuchs’ dystrophy is most common in people over the age of 60 in the United States. This progressive disease causes blurry vision as the cells in the cornea begin to die off, affecting the inner layer of the cornea, known as the endothelium.
This loss of the endothelium causes eye inflammation from fluid buildup. Everything may appear hazy, foggy, or blurry if you have Fuch’s dystrophy.
Implanting a donor or artificial cornea removes these cells that block light and restores sight. With Fuchs’ dystrophy, some patients may need Descemet’s Membrane Endothelial Keratoplasty (DMEK) or Descemet’s Stripping Automated Endothelial Keratoplasty (DSAEK).
DMEK and DSAEK are two different kinds of corneal transplants. With these transplants, they only replace the inner layer of the cornea with a donor endothelial layer.
Instead of needing a full corneal transplant, these advanced cornea procedures only replace what’s necessary for the cornea. For patients, this means less time spent recovering and better results.
Corneal Erosions
Corneal erosions can happen to people who have had eye injuries. For example, your child could accidentally scratch their eye, creating a corneal erosion. This accident may make them more likely to have spontaneous scratches in the future.
These marks are painful and may make the eye more sensitive to light. Blurry vision and wateriness are also common. Undergoing a corneal transplant removes the damaged cells and prevents future erosions.
Keratoconus
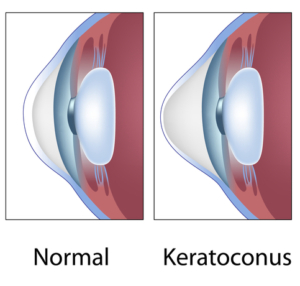
People who have keratoconus have a cornea that’s an irregular shape. Instead of being spherical, like a basketball or baseball, the cornea is closer in shape to a football when someone has keratoconus.
As keratoconus gets worse over time, the cornea may steepen and become thinner. Patients with the conditions usually receive a diagnosis in their teens or early twenties, which often affects both eyes.
This disease may be stable or worsen with age. In its early stages, patients can treat keratoconus using scleral contact lenses.
Some patients may also undergo a corneal cross-linking procedure that strengthens the cornea and prevents further keratoconus progression. Patients with severe keratoconus may need to undergo a corneal transplant to restore their vision.
Trichiasis
Trichiasis is a condition that occurs when the eyelashes grow toward the eye instead of away from the eye. The lashes can rub on the cornea causing painful scratches.
You may have vision loss if this condition goes untreated. A corneal transplant may be necessary to address abrasions on the surface of the eye.
What is a Corneal Transplant?
Corneal transplants are also called keratoplasties. This procedure uses donor tissue to replace the damaged or diseased cornea. The tissue comes from donors that are carefully screened before accepting them.
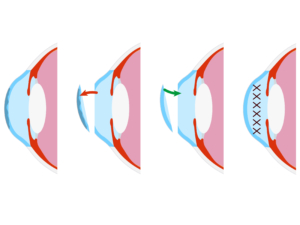
Penetrating Keratoplasty
Traditional cornea replacements are called penetrating keratoplasties or full-thickness cornea transplantation. During this procedure, your surgeon will remove the entire cornea and replace it with a donor cornea.
Endothelial Keratoplasty
An endothelial keratoplasty may help if you’ve damaged the endothelium of your cornea. The endothelium is the innermost layer of the cornea.
There are two kinds of endothelial keratoplasty procedures that a surgeon performs. These include a Descemet stripping automated endothelial keratoplasty (DSAEK) or a Descemet membrane endothelial keratoplasty (DMEK).
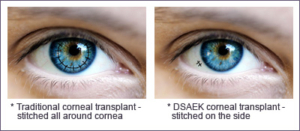
The most significant difference between the two procedures is the thickness of the donor corneas. With DSAEK, the donor cornea will be thicker, while with DMEK, it’s thinner.
The thickness of the corneal tissue depends on which kind of transplant procedure is best for your eyes.
Deep Anterior Lamellar Keratoplasty
With a deep anterior lamellar keratoplasty, only the middle and outer layer of the cornea are removed. This kind of corneal transplant is helpful for people with scratches or injuries to these layers.
Endothelial and anterior lamellar procedures may have a faster recovery and present lower risks. The procedures involve less removal of corneal tissue and do not require sutures.
Your eye doctor will decide between these corneal transplant procedures based on the location of damage to your eye. It is essential to know that there is the potential for complications with a corneal transplant.
Eye inflammation and bleeding are possible, and the development of glaucoma and cataracts—other risks to be on the lookout for include severe eye infection and refractive errors.
What to Expect Once You Know You Need a Corneal Transplant

If you need a corneal transplant, the first step is your surgeon will place you on a transplant list with an eye bank. It can take weeks or months for viable live tissue to become available.
Some people prefer to be awake when they have their cornea transplant. If you choose this option, you’ll have local anesthesia to numb the eye and surrounding area. You may also choose to be put under and be asleep.
Before the corneal transplant begins, a speculum will be placed in your eye to keep your eyelid open. If you are getting a traditional corneal transplant surgery, the surgeon will remove a circular area of the cornea.
They replace the tissue with the donor cornea and suture it into place. These stitches stay in your eye for about a year after the transplant. Your surgeon will then place a plastic shield over the eye to protect it and encourage healing.
This outpatient procedure may take several hours. You will need a ride home as you may be sensitive to light or a little sleepy after the anesthesia.
Those who have an endothelial keratoplasty undergo a less invasive procedure. During an endothelial keratoplasty, the surgeon creates a small incision in the eye.
After making this incision, they insert the thin donor tissue on the back of the cornea. With this tool, they create an air bubble that moves the endothelial layer into the correct place.
The opening will heal itself without stitches or adhesives. You will need someone to drive you home.
Corneal transplant recipients may use eye drops and medications to reduce inflammation and prevent infections. It is critical to follow your eye doctor’s directions on these medications to avoid cornea rejection.
Are you looking for more information about corneal transplants? Schedule an appointment at Eye Consultants of North Dakota in Fargo, ND, with our cornea specialist Dr. Anne Keating!



